When a medical claims management is adjudicated, the health insurance provider evaluates it before deciding whether to accept it or reject it. Cross-analysis of the patient\'s benefits and coverage details is used to accomplish this. Medical billing automated claim adjudication streamlines A/R administration and follow-up procedures by providing quick, hassle-free access to comprehensive claim adjudication status data. Healthcare auto adjudication software can be developed to automate the follow-up process for Medicaid and payers, shortening the time it takes for a provider to get paid while lowering the cost-to-collect.
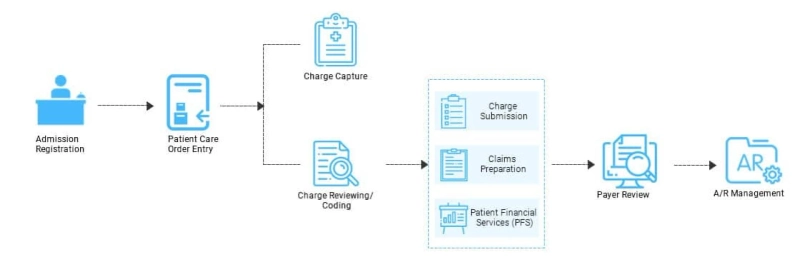
Healthcare organizations can obtain up-to-date data on active claims to quickly make educated decisions. To follow up on outstanding claims issues and gain the option to timely appeal refused claims hassle-free, healthcare claims adjudication procedure steps can be implemented. Healthcare organisations can effectively create follow-up procedures to maximise recovery by analysing denial rates and coding errors. In order to comply with strict federal rules and combat the rising rate of medical claims denial, customised healthcare claims management software solutions might be extremely helpful. To automate your healthcare claim management processing workflow throughout a claim\'s life cycle, custom healthcare solutions seamlessly combine a variety of complicated systems, platforms, and human processes.
One persistent annoyance of the U.S. healthcare claims adjudication process is the practise of dealing with a sizable amount of paperwork that arrives in bits and pieces and needs to be assembled and laboriously submitted. Through a lighter financial burden, automated healthcare solutions have the potential to bring happiness to all parties involved in the healthcare sector. It lessens the requirement for manual processing as well. The programme can access accounts and open cases thanks to quality execution, which lowers the cost of insurance policies and claims management in healthcare. Fraud detection and recoverable monitoring are further benefits. These solutions can be implemented on a cutting-edge platform and use a wide range of deep learning algorithms to dramatically improve the process of risk and fraud analysis. software for advanced claims adjudication.