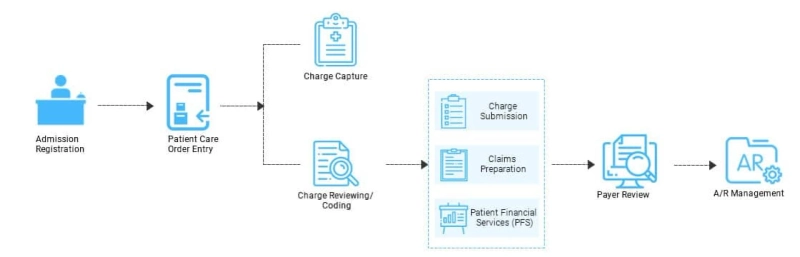
The electronic submission of claims, where automated systems can prepare, verify, and submit claims electronically, optimises the flow chart for adjudicating medical claims management. The necessity for manual paperwork is eliminated as a result. The use of electronic documentation and records improves accessibility. Real-time access to both past and present claims, as well as regions that need to be examined, is provided by high-performance software. Finally, real-time professional claim adjudication is possible with engaging, transactional interactions.
Software used to adjudicate medical claims should be updated frequently to better serve all parties involved in the healthcare sector. Optical Character Recognition (OCR) is one such feature that has a great potential to reduce the likelihood of major errors in coding and claim submission. Document scanning, electronic programming, and isolation are used to accomplish this. The advantages are infinite, from the ease of electronic data interchange entry using mHealth technologies through validation through technology to the flexibility of errors being identified prior to submission. Through automated health systems, every customised offer of claims management healthcare boosts revenue, streamlines the procurement process, and increases retention rates.
One persistent annoyance of the U.S. healthcare claim management adjudication process is the practise of dealing with a sizable amount of paperwork that arrives in bits and pieces and needs to be assembled and laboriously submitted. Through a lighter financial burden, automated healthcare solutions have the potential to bring happiness to all parties involved in the healthcare sector. It lessens the requirement for manual processing as well. The programme can access accounts and open cases thanks to quality execution, which lowers the cost of insurance policies and medical claims. Fraud detection and recoverable monitoring are further benefits. These solutions can be implemented on a cutting-edge platform and use a wide range of deep learning algorithms to dramatically improve the process of risk and fraud analysis. The entire lifespan may be streamlined with sophisticated claims adjudication software.