Learn about PMDD treatment options, including medical, natural, and lifestyle approaches to relieve symptoms and improve emotional balance effectively.
Premenstrual Dysphoric Disorder (PMDD) is a severe form of premenstrual syndrome that affects mood, energy, and physical well-being. While PMS is common, PMDD symptoms can significantly interfere with daily life, relationships, and mental health. Understanding the causes and finding the right PMDD treatment is essential for long-term relief and emotional stability.
What Is PMDD and Why Does It Happen?
PMDD is linked to hormonal changes during the luteal phase of the menstrual cycle. This phase occurs after ovulation and before menstruation begins. People with PMDD experience an exaggerated response to normal hormonal fluctuations, especially in serotonin levels.
Common emotional and physical symptoms include:
- Intense mood swings and irritability
- Depression or anxiety
- Fatigue and low motivation
- Difficulty concentrating
- Sleep disturbances
- Physical pain such as cramps, bloating, and breast tenderness
While the exact cause remains unclear, genetic predisposition, stress, and lifestyle factors can all play a role
Types of PMDD Treatment: Medical, Natural, and Lifestyle Options
When searching for the best PMDD treatment, it’s important to know that solutions vary based on individual needs. A combination of medical and natural approaches often works best.
1. Medical Treatments
Common medical options include:
- SSRIs (Selective Serotonin Reuptake Inhibitors): These antidepressants, such as fluoxetine or sertraline, help balance serotonin and reduce mood-related symptoms.
- Hormonal Therapies: Birth control pills, especially those with drospirenone, can stabilize hormonal fluctuations.
- GnRH Agonists: In severe cases, these medications temporarily suppress ovarian hormone production.
- Pain Relievers: NSAIDs like ibuprofen help with cramps and bloating.
A healthcare provider can guide the best medical route based on symptom intensity and medical history.
2. Natural Remedies and Nutritional Support
Natural remedies can complement medical PMDD treatments and support overall hormonal balance.
Effective natural approaches include:
- Magnesium and Calcium: Help regulate mood and reduce cramps.
- Vitamin B6: Supports serotonin production and energy.
- Chasteberry (Vitex Agnus-Castus): May balance estrogen and progesterone.
- Omega-3 Fatty Acids: Reduce inflammation and improve mood.
- Herbal Teas: Chamomile or green tea can ease anxiety and bloating.
Always consult a doctor before starting supplements to ensure safety with other medications.
3. Lifestyle Adjustments That Make a Difference
Lifestyle changes can have a strong impact on PMDD symptom control.
Practical tips include:
- Regular Exercise: Even 30 minutes of daily activity boosts endorphins.
- Balanced Diet: Focus on whole foods, lean proteins, and fiber while reducing sugar and caffeine.
- Sleep Hygiene: Maintain a consistent sleep schedule for hormonal regulation.
- Mindfulness Practices: Meditation, journaling, or deep-breathing exercises reduce stress.
- Limit Alcohol and Smoking: Both can worsen emotional and physical symptoms.
These adjustments not only reduce PMDD symptoms but also improve overall well-being.
The Role of Mental Health Support in PMDD Treatment
PMDD deeply affects emotional stability, relationships, and self-esteem. Therefore, therapy plays a key role in recovery.
Helpful approaches include:
- Cognitive Behavioral Therapy (CBT): Helps manage negative thought patterns.
- Dialectical Behavior Therapy (DBT): Useful for emotional regulation.
- Support Groups: Sharing experiences reduces feelings of isolation.
- Stress Management Techniques: Yoga, guided imagery, or progressive relaxation can ease emotional strain.
Combining therapy with medical or holistic treatments often produces the best results.
How Diet and Gut Health Influence PMDD
Nutrition affects hormone metabolism, inflammation, and mood regulation—all central to PMDD management. A gut-friendly diet can enhance serotonin production, since much of it originates in the gut.
Key dietary strategies:
- Eat fiber-rich foods like oats, lentils, and vegetables.
- Include probiotic foods such as yogurt, kefir, and sauerkraut.
- Avoid processed and high-sodium meals that can trigger bloating.
- Stay hydrated throughout the day.
Tracking food intake and symptoms can help identify specific triggers.
Sleep and Stress: Hidden Drivers of PMDD Symptoms
Chronic stress and poor sleep amplify PMDD symptoms by disrupting hormonal balance and serotonin production.
To improve both:
- Keep a consistent bedtime routine.
- Avoid screens 30 minutes before bed.
- Create a calm sleep environment with soft lighting and cool temperature.
- Practice daily relaxation methods like meditation or stretching.
Small, consistent changes can significantly improve energy and mood stability.
Exercise as a Form of PMDD Treatment
Exercise helps regulate hormones, improve blood flow, and enhance serotonin and endorphin levels—all of which help with PMDD management.
Recommended exercises:
- Cardio: Walking, cycling, or swimming.
- Strength training: Helps maintain muscle tone and reduce fatigue.
- Yoga and Pilates: Encourage relaxation and flexibility.
Consistency matters more than intensity; moderate daily activity provides the most benefits.
Long-Term PMDD Management and Monitoring
PMDD is a chronic condition for many, but ongoing monitoring can help reduce flare-ups.
Keeping a daily symptom journal allows individuals to track emotional and physical changes, correlate them with the menstrual cycle, and identify patterns.
Helpful tools:
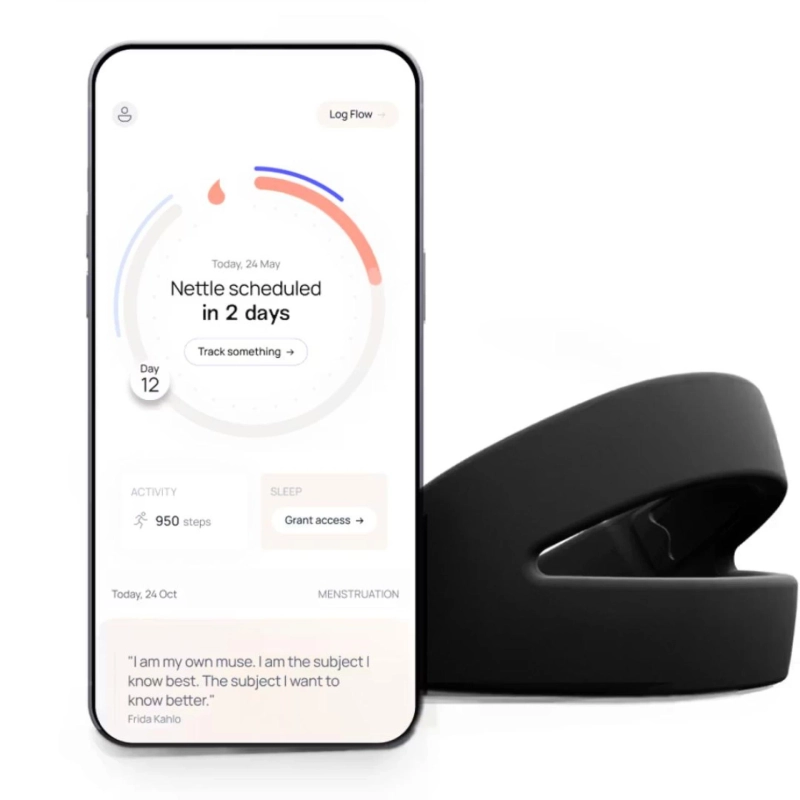
- Cycle-tracking apps
- Mood charts
- Symptom logs for triggers like stress, diet, or sleep
These insights help healthcare providers adjust treatments and enhance quality of life.
When to Seek Professional Help
If PMDD symptoms disrupt work, relationships, or emotional health, professional evaluation is crucial. A gynecologist or psychiatrist familiar with hormonal mood disorders can assess whether the condition requires medication, therapy, or both.
Prompt treatment can prevent worsening depression and anxiety, leading to more stable daily functioning.
Frequently Asked Questions
What is the most effective PMDD treatment?
The most effective treatment combines SSRIs, hormonal birth control, and lifestyle changes tailored to each individual’s needs.
Can diet changes really help PMDD?
Yes. Reducing sugar, caffeine, and processed foods while increasing whole grains, lean proteins, and omega-3s can improve hormone balance and mood.
Is PMDD the same as PMS?
No. PMDD is more severe and includes significant mood symptoms like depression and anger that interfere with daily life.
How long does PMDD last?
Symptoms typically begin one to two weeks before menstruation and end shortly after the period starts.
Can therapy help with PMDD?
Yes. Cognitive Behavioral Therapy (CBT) and stress management techniques are highly effective for emotional regulation and coping strategies.
Can PMDD go away naturally?
In some cases, symptoms lessen with age or after hormonal changes like menopause, but many benefit from consistent treatment and lifestyle support.