Safety pharmacology (safety pharmacology) research is an important part of the non-clinical safety evaluation of new drugs when the dose of the main research drug is within the therapeutic range or above the therapeutic range. There are potential undesired adverse effects. And observed in the study / or speculated adverse drug reaction mechanism so as to maximize the protection of new drugs before entering clinical research or after marketing early detection of possible adverse reactions beyond the therapeutic effect.
When some adverse reactions to humans and animals are observed or speculated in other non-clinical trials and clinical trials, safety pharmacology research should be added and supplemented. The objectives of safety pharmacology research include: ① determine the undesired pharmacological effects of drugs that may be related to human safety; ② evaluate the adverse drug reactions and (or) pathophysiology of drugs observed in toxicology and (or) clinical research ③ observed and (or) speculated adverse drug reaction mechanism. Safety pharmacology research runs through the whole process of new drug research and can be carried out in stages.
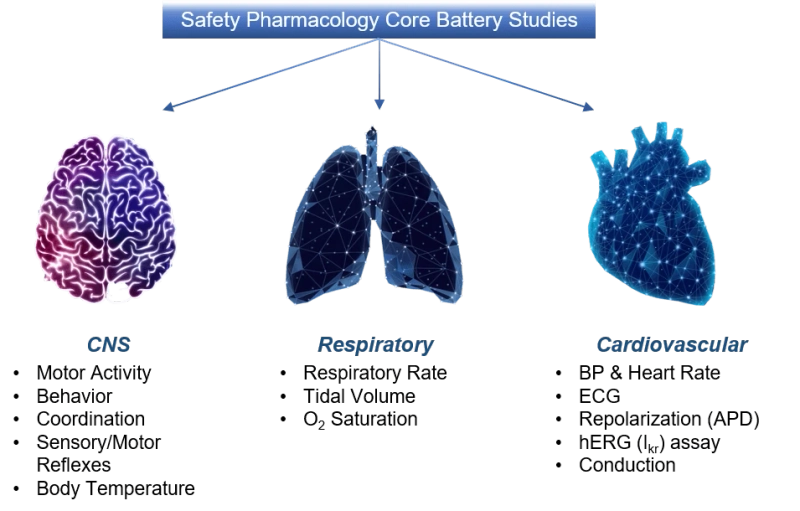
The International Council for Harmonization of Technical Requirements for Registration of Drugs for Human Use (ICH) issued corresponding guidelines for the evaluation of safety pharmacology tests, which were formulated by the corresponding ICH expert groups according to the ICH procedures, and have now been adopted by the European Union, Japan and the United States. We can provide safe pharmacological experiment services using large and small animals to explore the effects of drugs on central nervous system, respiratory system and cardiovascular system, and to support drug R&D.
The name and introduction of ICH guidelines
At present, ICH\'s non-clinical research evaluation and risk assessment of drug safety and pharmacology mainly include "ICH S7A: Guidelines for Human Drug Safety Pharmacology Research" (ICHS7A) and "ICHS7B: Human Drug Delayed Ventricular Repolarization (QT Interval Prolongation) Guidelines for Nonclinical Evaluation of Potential Effects (ICH S7B) two guidelines.
ICHS7A, currently in Phase 4 of the ICH process, provides definitions, general principles and recommendations for safety pharmacology studies. This principle generally applies to new chemical entities for human use and biotechnology products. In some cases (such as when clinical adverse reactions occur, new drug populations or new routes of administration cause new safety concerns), it may also be applicable to marketed drugs.
ICHS7B is also currently in Phase 4 of the ICH process. ICHS7B is a supplement and extension to ICH S7A, and its main content is non-clinical research strategies to evaluate the potential role of test substances in delaying ventricular repolarization. This guideline applies to new compounds for human use, as well as marketed drugs (such as clinical adverse events, new drug populations, or addition of new routes of administration that have not been used before).
"ICH S7A: Guiding Principles for Safety Pharmacology Research of Drugs for Human Use"
This guideline recommends a framework for core combination trials, supplementary trials, and follow-up trials. Among them, the core combination of safety pharmacology tests consists of three parts, namely the central nervous system, cardiovascular system and respiratory system. Major areas of study of the central nervous system include motor function, behavioral changes, coordination, sensory or motor reflexes, and body temperature. Functional combination test (FOB), modified Irwin\'s test and other methods can be used.
Cardiovascular system studies mainly include blood pressure, heart rate, and electrocardiogram. In vivo, in vitro, and/or ex vivo evaluation methods including repolarization and conduction abnormality test methods should also be considered. The respiratory system includes things like respiratory rate, gas volume, or hemoglobin oxygen saturation. Clinical observation of animals is generally not suitable for evaluating respiratory function, and appropriate methods need to be used to quantify these indicators of respiratory function.
"ICHS7B: Guidelines for Nonclinical Evaluation of Potential Effects of Human Drugs on Delaying Ventricular Repolarization (QT Interval Prolongation)"
Toxicity of developmental compounds and drugs is one of the leading causes of development interruptions or withdrawal of drugs from the market. Among them, drug-induced arrhythmia and liver toxicity are the most common, and early assessment of these risks is crucial to ensure the success of research and development.
According to the ICHS7B guidelines, for more than ten years, the preclinical cardiac safety evaluation has mainly been to detect the inhibitory effect of the research and development compounds on the hERG ion channel and the effect on the QT interval of the animal electrocardiogram. Although these tests have effectively avoided the listing of drugs with the risk of TdP, due to the oversimplification, high sensitivity, and lack of specificity of these tests, false positive results may be caused, resulting in interruption of research and development, thereby affecting the process of new drug development.
In the development of new drugs, the risk of the cardiovascular system is often discovered in the clinical stage; ICH E14 has made strict requirements for TQT (a thorough clinical QT assay) research, setting a very sensitive risk threshold (~2% QT increase – very small!). Cardiac safety poses a risk that cannot be ignored in the late stage of new drug development.
The implementation of ICH S7B, especially E14, the results are eye-catching and warm: in the TQT research submitted to the FDA, the proportion of drugs with QT prolongation dropped from 60% in 2005 to 10% in 2012, and new drugs approved for marketing at the same time , and there are few accidental occurrences of TdP1,2,3. In the process, the core experiments established by the S7B guidelines (in vitro hERG and in vivo heart-rate corrected QT--QTc assays) were inevitably ignored by regulatory authorities and clinical medical workers. Excessive emphasis and reliance on TQT has greatly wasted R&D resources, increased the cost of drug R&D, and even delayed the drug R&D process. On March 2020, a group of pharmaceutical giants jointly published an article, pointing out the importance of core experiments in S7B.
With the further recognition and emphasis of the core experiments established by ICH S7B, it becomes imperative to clarify some issues (such as: best practice paradigm). So S7B Q&A took advantage of the trend.
S7B Q&A can be roughly divided into three parts.
- Integrated Risk Assessment -- Integrated Risk Assessment (S7B Q&As 1.1–1.2)
This section presents points to be considered in order to be able to effectively apply nonclinical data to clinical research. First of all, in this part, the principle of defining negative in vitro hERG and in vivo QTc assays is clarified, involving factors such as safety window, detection concentration range and best practice; secondly, it describes in detail how to calculate hERG safety margin; and then explore how non-clinical experimental data can support the design and understanding of clinical experiments in double-negative and non-double-negative scenarios. It is proposed that when the experimental results are inconsistent or it is difficult to understand the results of non-clinical experiments, additional experiments can be used for further mechanism exploration and TdP risk assessment.
At the same time, it is pointed out that if applicable, the evaluation of other ion channels should also follow the best practice recommended by S7B Q&A 2.1-Best practice.
- Best Practice Paradigm -- Best Practice Considerations for In vitro Studies and In vivo QT Studies provides a detailed description of the core experiments and the best practices of iPS-CM Repolarization Assays.
- Application principles of arrhythmia models -- Principles of Proarrhythmia Models When the core experiment is not double-negative, the arrhythmia model can be used as an additional experiment to evaluate the risk. These models cover various categories such as in silico, in vitro, ex vivo, and in vivo. This part introduces the six application principles of the arrhythmogenic model and the general use process, which provides the basis for the more detailed specification of Stage-2.
ICH S7B summary:
The current ICH S7B/E14 guidelines focus on the evaluation of drug-induced ventricular repolarization delay, such as hERG ion channel blockade and ECG QT interval prolongation; there is no direct assessment of the main clinical problem endpoint, namely ventricular rhythm Risk of malfunction (i.e. TdP).
The success of ICH S7B/E14 is that after the release of these two guidelines, no TdP-related drugs have been withdrawn from the market. However, the problem brought by ICH S7B/E14 is that many compounds block hERG ion channels and prolong the QT interval of ECG, but do not cause arrhythmia. For these compounds, screening against the hERG ion channel could lead to unnecessary R&D interruptions; or once marketed, these drugs would be labeled and the drug\'s use limited.