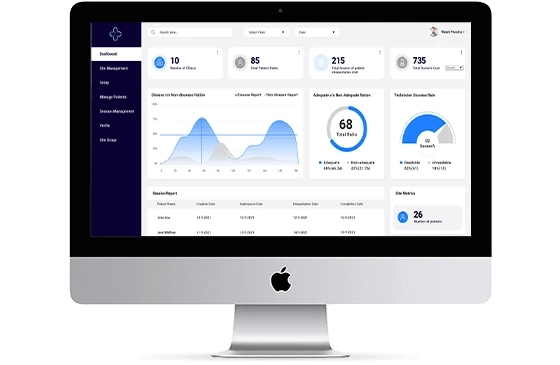
Overcoming Challenges for Denial Management to Eliminate Payer Denials
In the modern era, maintaining denial appeal management software in medical billing has become a challenging task. Hospitals and medical workers may suffer a ...

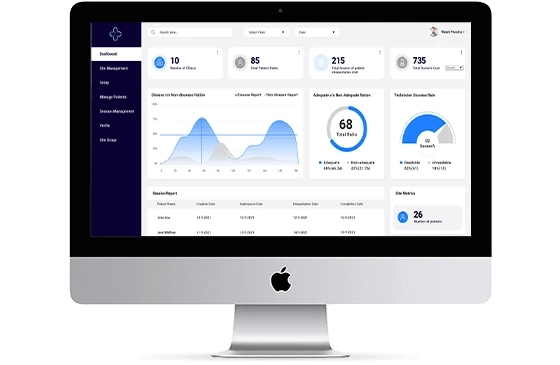
In the modern era, maintaining denial appeal management software in medical billing has become a challenging task. Hospitals and medical workers may suffer a ...