Pain and inflammation affect daily life in ways that often feel confusing and frustrating. You may experience joint stiffness, chest discomfort, muscle aches, headaches, or persistent fatigue without a clear cause. Many people focus on the affected body part and miss an important factor that shapes how pain develops and settles: gut health.
I write this article as both a medical professional and a content strategist who works closely with patient-focused education. I aim to explain how your gut influences pain and inflammation in clear, practical terms. I also address common questions you may already have, especially if you live with long-term inflammatory conditions or unexplained pain.
Why gut health matters more than digestion
Most people associate the gut with digestion alone. In reality, the gut acts as a control centre for immune activity, inflammation, and pain signalling.
Your digestive tract houses trillions of bacteria, fungi, and other microorganisms. Together, they form the gut microbiome. These organisms help digest food, produce vitamins, and protect against harmful microbes. They also communicate with your immune system and nervous system every day.
When the gut stays balanced, your body manages inflammation efficiently. When that balance breaks down, inflammatory signals can increase and pain sensitivity may rise.
The gut–immune connection and inflammation
Around 70 per cent of your immune cells sit in or around the gut. This means the gut directly shapes immune responses throughout the body.
A healthy gut lining acts as a selective barrier. It allows nutrients to pass through while keeping toxins and harmful bacteria out of the bloodstream. When the gut lining becomes irritated or weakened, unwanted substances can cross into circulation. Many people refer to this process as increased intestinal permeability.
Once this happens, the immune system reacts. It releases inflammatory chemicals such as cytokines. These chemicals do not stay localised. They travel through the body and can affect joints, muscles, nerves, and connective tissue.
Over time, this low-grade inflammation may contribute to chronic pain conditions.
How gut imbalance increases pain sensitivity
Inflammation alone does not explain all pain experiences. The gut also influences how strongly you feel pain.
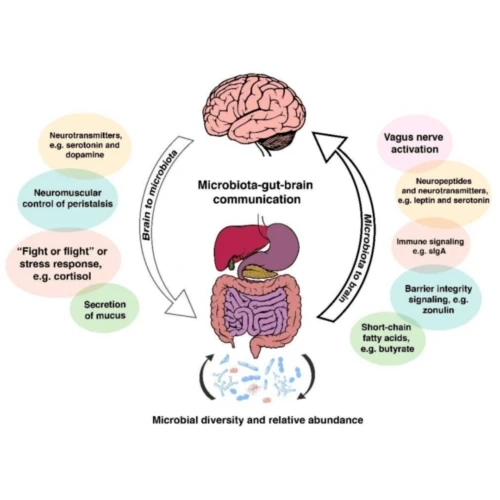
The gut communicates with the brain through the gut–brain axis. This two-way communication uses nerves, hormones, and immune signals. When gut bacteria fall out of balance, pain signals may amplify.
You may notice:
- Heightened sensitivity to pressure or movement
- Pain flares without obvious triggers
- Slow recovery after minor strain or injury
Certain gut bacteria help produce short-chain fatty acids. These compounds calm inflammation and support nerve function. When beneficial bacteria decrease, pain regulation may suffer.
Chronic pain conditions linked to gut health
Research increasingly links gut health to several pain-related conditions. While each condition has unique features, gut imbalance often plays a supporting role.
Joint and muscle pain
Inflammatory joint pain often appears alongside digestive symptoms such as bloating, reflux, or irregular bowel habits. Inflammation triggered in the gut can worsen stiffness and swelling elsewhere.
Chest wall pain and costochondral discomfort
Inflammation of cartilage connecting the ribs to the breastbone may feel alarming. Many people focus on posture or strain alone. Gut-driven inflammation may also contribute. Some readers explore related topics such as Costochondritis Natural Supplements while learning how inflammation behaves systemically.
Headaches and migraines
The gut produces many neurotransmitters involved in pain processing, including serotonin. Gut imbalance can disrupt this production and increase headache frequency.
Widespread pain and fatigue
Conditions involving body-wide discomfort often coincide with gut issues. Immune activation originating in the gut may contribute to persistent pain signals.
Food, inflammation, and pain pathways
Food choices strongly influence gut health. What you eat shapes the composition of your gut microbiome within days.
Foods that support a calmer gut
- Fibre-rich vegetables and fruits
- Fermented foods such as yoghurt, kefir, and sauerkraut
- Whole grains that feed beneficial bacteria
- Healthy fats from olive oil, nuts, and seeds
These foods encourage bacteria that reduce inflammation and support gut lining integrity.
Foods that may worsen inflammation
- Ultra-processed foods
- Excess refined sugar
- Frequent alcohol intake
- Certain additives and emulsifiers
These foods may irritate the gut lining and promote inflammatory bacteria.
You do not need extreme restriction. Small, consistent changes often produce better results.
The role of stress and the gut–pain cycle
Stress affects gut health directly. When stress levels remain high, digestive function changes. Blood flow shifts away from the gut, digestion slows, and gut bacteria composition may alter.
This creates a cycle:
- Stress disrupts gut balance
- Gut imbalance increases inflammation
- Inflammation heightens pain sensitivity
- Pain increases stress
Breaking this cycle often requires addressing both gut health and stress management.
Simple practices such as paced breathing, regular meals, and adequate sleep can support gut resilience.
Gut health and inflammatory chemicals
The body uses chemical messengers to regulate inflammation. Some of these chemicals promote healing, while others amplify pain.
A balanced gut encourages the production of anti-inflammatory compounds. An imbalanced gut may trigger excessive production of pro-inflammatory molecules.
This difference influences:
- Joint swelling
- Muscle soreness
- Nerve irritation
- Recovery after injury
Supporting gut health may help shift this chemical balance.
Gut bacteria and nutrient absorption
Pain management often focuses on nutrients such as magnesium, vitamin D, and B vitamins. Absorption of these nutrients depends heavily on gut function.
If gut health suffers, even a well-planned diet may not deliver the nutrients your body needs to regulate inflammation and nerve signalling.
Some people research Natural Remedies for Costochondritis and similar topics while learning that gut support may improve how the body uses supportive nutrients.
The connection between gut health and autoimmune pain
Autoimmune conditions involve immune attacks on the body’s own tissues. Many autoimmune disorders also include chronic pain.
Gut imbalance may influence autoimmune activity by:
- Increasing immune activation
- Altering immune tolerance
- Promoting inflammatory signalling
While gut support does not replace medical care, it may complement existing management strategies.
Probiotics, prebiotics, and pain modulation
Probiotics introduce beneficial bacteria. Prebiotics feed existing good bacteria. Together, they shape gut balance.
Certain probiotic strains may help reduce inflammation and improve pain thresholds. Results vary between individuals, so responses may differ.
You may notice gradual changes rather than immediate relief. Consistency matters more than high doses.
Supplements and gut-focused support
Some people explore targeted supplements to support gut health and inflammation balance. These may include:
- Omega-3 fatty acids
- Curcumin
- Zinc
- Glutamine
Quality and sourcing matter. Many readers search for reliable options such as Best Vitamins and Supplements Products Online UK to ensure safety and consistency.
Always discuss supplements with a healthcare professional, especially if you take medication or manage a chronic condition.
Gut health, medication, and pain relief
Pain medications can affect gut health. Non-steroidal anti-inflammatory drugs may irritate the gut lining with frequent use. Antibiotics can disrupt gut bacteria balance.
Supporting gut health during medication use may reduce digestive side effects and support long-term wellbeing.
Simple steps include spacing medications appropriately with meals and focusing on gut-friendly foods.
Signs your gut may influence your pain
You may suspect a gut–pain link if you notice:
- Digestive discomfort alongside pain flares
- Pain worsening after certain foods
- Frequent bloating or reflux with joint or muscle pain
- Fatigue linked to digestive symptoms
These signs do not replace medical assessment but may guide supportive strategies.
Practical steps to support gut health for pain management
You can begin supporting gut health without drastic changes.
Build regular meal patterns
Eating at consistent times supports digestive rhythm and gut signalling.
Increase fibre gradually
Sudden fibre increases may cause discomfort. Gradual changes allow gut bacteria to adapt.
Stay hydrated
Water supports digestion and nutrient transport.
Prioritise sleep
Sleep influences gut bacteria composition and immune balance.
Move gently
Regular movement supports digestion and reduces inflammation.
Setting realistic expectations
Gut health support does not offer instant pain relief. Changes often occur over weeks rather than days.
Some people notice improved digestion first, followed by subtle reductions in pain intensity or frequency. These shifts may feel small but can add up over time.
Working with healthcare professionals
Gut health strategies work best alongside professional guidance. A healthcare provider can rule out serious conditions and help tailor dietary or supplement approaches.
Pain deserves careful evaluation. Gut support complements, rather than replaces, medical care.
Bringing it all together
Pain and inflammation rarely arise from a single cause. The gut influences immune activity, nerve signalling, nutrient absorption, and inflammatory balance throughout the body.
By supporting gut health, you may reduce inflammatory load and improve how your body processes pain signals. This approach fits well alongside conventional care and lifestyle adjustments.
If you live with persistent pain, consider looking beyond the painful area itself. The gut may play a quieter yet significant role in how your body feels each day.