Gut flora and metabolites influence these diseases
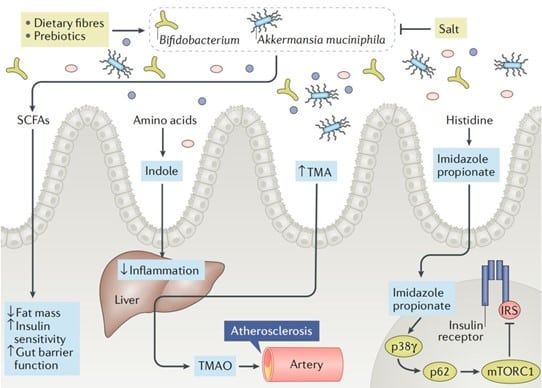
Over the past 15 years, numerous studies have linked obesity, type 2 diabetes (T2DM), and cardiovascular disease to specific changes in gut microbiota composition and function. However, most studies focus on fatty acids (such as short-chain fatty acids), and some involve sugar, dietary fiber, prebiotics, etc. Over the past 5 years, it has been documented that microbial conversion of some food components such as carnitine, choline, or lecithin to produce trimethylamine N-oxide (TMAO) promotes atherosclerosis in rodent models. occurrence and is closely related to increasing the risk of cardiovascular disease in humans (Figure 1).
Based on these data, metabolites produced by microorganisms are considered to be key metabolic regulators that can affect different organs throughout the body and ultimately produce a range of beneficial or harmful functions. In addition to TMAO, which may be a potential key molecule, other microbial metabolites, such as aromatic amino acids, may also be involved in anti-inflammatory processes in the liver (Figure 1); however, only a few studies have clearly dissected specific microbially derived amino acid metabolites Molecular mechanisms leading to disease. The MetID team of Medicilon is composed of experienced scientists. We provide fast and reliable in vivo and in vitro MetID and reactive metabolite capture services. We also support new drug screening and domestic and oversees IND filings. Since the establishment of MetID team, Medicilon has successfully completed multiple different types of research projects for clients, including challenging peptide MetID research.
Figure 1 New mechanisms linking microbial-derived molecules and metabolism
A 2018 study by Ara Koh and colleagues described how metabolites produced by microbes contribute to disease. They found that imidazole propionate, produced from histidine, is an important microbial metabolite that promotes the development of insulin resistance and ultimately leads to T2DM. Using untargeted metabolomics analysis, the portal vein plasma of obese T2DM patients was compared with the plasma of non-T2DM patients matched by BMI. It was found that the levels of four amino acid metabolites in the plasma of T2DM patients were higher than those of the control group. The team then cross-validated this link with the microbiota, demonstrating that imidazole propionate was the only metabolite whose levels were increased in regular mice, germ-free mice, or antibiotic-treated mice. In a second cohort of 649 people, Koh and colleagues demonstrated that early-treatment T2DM patients had higher levels of imidazole propionate than subjects with normal glucose tolerance.
In this study, the author combined in vitro models and animal models to analyze the molecular mechanism of imidazole propionate involved in glucose dysregulation: this component will impair the ability of cells to respond correctly to insulin, thereby triggering insulin resistance and ultimately leading to T2DM. Therefore, imidazole propionate was determined to be an inhibitor of the intracellular insulin receptor signaling cascade. At the same time, imidazole has been shown to act as an activator of the p38γ-p62-mTORC1 pathway, which can inhibit the formation of the insulin receptor substrate protein and mTORC1 complex (Figure 1).
In addition to more classic metabolite studies, high salt intake has also been associated with cardiometabolic risks and metabolic disorders. So far, most research on this topic has dealt with the role of this particular mineral and its impact on heart disease and obesity.
As we all know, salt has been used for thousands of years to prevent the growth of microorganisms (such as pickling and preserving food). In a 2018 article, El Hadji Seck and colleagues examined the relationship between salt intake, gut microbiota composition, and obesity.
In a geographically diverse group of more than 1,300 individuals, they discovered a potentially unexpected link between salt and microbiota. First, they found that fecal salinity increased in obese people in different countries, and that high salinity could even be used as a predictor of obesity, regardless of age, gender, and country.
Additionally, they found a dose-dependent relationship between fecal salinity and body weight, suggesting a link between intestinal salinity levels and obesity. The authors used both 16S sequencing methods and culturomics methods to study halophilic bacteria. The study included the analysis of 572 samples and the culture of more than 85,000 microbial colonies, prompting the discovery of new bacterial and archaeal species. In addition, 16S sequencing analysis of 164 samples showed an inverse relationship between salinity and microbial diversity. Therefore, both approaches (high-throughput sequencing and culturomics) help to demonstrate that the composition of the gut microbiota is not only related to obesity but also to salinity.
The authors also found that in addition to the enrichment of halophilic bacteria, fecal salinity was a key factor in the reduction of Bifidobacterium and Akkermansia muciniphila. Both bacteria are inversely associated with metabolic disorders, low-grade inflammation, insulin resistance, and T2DM. In addition, they are producers of SCFAs. These microbial metabolites are involved in regulating multiple targets such as glucose, lipid and energy metabolism, as well as immunity and cancer.
Bifidobacteria and A. muciniphila are probiotics, microorganisms that are beneficial to the health of the host. This study highlights that excessive salt intake can play an important role in the balance of the gut microbiota by reducing the levels of probiotic bacteria. The authors also discovered a novel mechanism by which salt may contribute to the development of metabolic diseases associated with obesity.
Another study in 2018 on Bifidobacterium and A.muciniphila found that a strain of Bifidobacterium has an improvement effect on obesity.
In a randomized, double-blind, placebo-controlled trial, Anna Pedret and colleagues found that after three months of taking live or heat-inactivated Bifidobacterium animalis subspecies lactis CECT 8145, fat biomarkers in obese people Improvements in levels (including reductions in body mass index (BMI) and visceral fat content) were seen, particularly in women. In addition, the authors also emphasized that the intake of live bacteria is associated with an increase in the number of A.muciniphila.
However, based on these results, it is difficult to determine whether the increase in A. muciniphila numbers is related to the observed phenotype, as the authors only observed a beneficial effect of high-temperature-inactivated B. animalis on visceral fat content, and in these experiments, A . muciniphila numbers did not increase. In addition, microbial metabolites were not investigated in this study. Therefore, it remains to be determined whether there are differences in the effects of supplementation with live or high-temperature-killed bacteria on host metabolism.
More and more researchers are beginning to explore the connection between microbiota, metabolites and host metabolism, and these articles in 2018 also discovered some interesting new mechanisms based on original research, which also link specific microorganisms to Or microbial metabolites are associated with the occurrence of some metabolic disorders.
In studies on humans, new mechanisms have gradually confirmed previous clinical findings.
Moreover, in addition to some more classic metabolites such as short-chain fatty acids, the effects or effects of amino acids or salts and other substances on microorganisms and microbial metabolites have also been gradually discovered, which has also provided a wider range of disease prevention measures and even improvements in treatment options. theoretical basis.
