Innovative technologies that enable individualized auditing strategies can be used to combat the medical claims management market\'s fierce competition. the ability to incorporate claims data through the adjudication of health insurance claims and develop a profile that focuses on the problematic areas and simplifies the entire lifecycle. The time-consuming and mostly unproductive traditional underwriting procedure is reduced by integrated care management. Health insurance claim adjudication can simplify income generating. Without intrusive questioning, the automation feature can notify the organizations about claims that are likely to be rejected. By automating routine chores like manual data entry, medical professionals can instead concentrate on sophisticated analytics and oversight procedures like population health management.
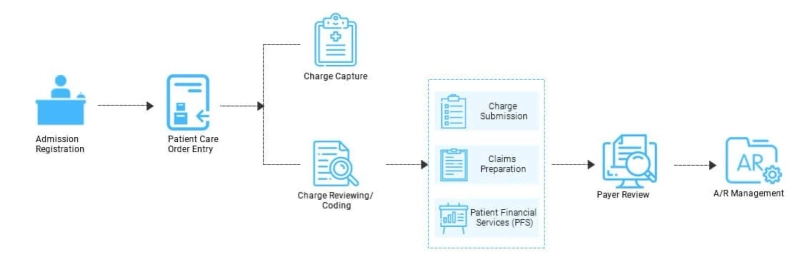
The electronic submission of claims, where automated systems can prepare, verify, and submit claims electronically, optimises the flow chart for adjudicating claims management in healthcare. The necessity for manual paperwork is eliminated as a result. The use of electronic documentation and records improves accessibility. Real-time access to both past and present claims, as well as regions that need to be examined, is provided by high-performance software. Finally, real-time professional claim adjudication is possible with engaging, transactional interactions.
Software used to adjudicate medical claims should be updated frequently to better serve all parties involved in the healthcare sector. Optical Character Recognition (OCR) is one such feature that has a great potential to reduce the likelihood of major errors in coding and claim submission. Document scanning, electronic programming, and isolation are used to accomplish this. The advantages are infinite, from the ease of electronic data interchange entry using mHealth technologies through validation through technology to the flexibility of errors being identified prior to submission. Through automated health systems, every customised offer of claims management healthcare boosts revenue, streamlines the procurement process, and increases retention rates.