Precision-engineered biological therapies are replacing broad-spectrum interventions in the present oncology landscape, which is undergoing a profound change. CAR NK cell therapy, a sophisticated type of immunotherapy, lies at the forefront of this shift as it has advanced from lab theory to a practical experimental therapeutic option for an expanding variety of cancers.
To close the gaps in safety, speed, and accessibility, current research has shifted toward modified NK cells, in contrast to the early days of adoptive cell transfer, which concentrated almost entirely on T cells.
To navigate the future of cancer care, patients considering advanced choices must comprehend the workings of these "first responders" and their current trial status. Read on to learn what makes CAR t cell therapy a successful, experimental treatment option.
CAR-NK vs CAR-T: Redefining the Safety Profile
CAR-NK vs. CAR-T is a key comparison in contemporary immunotherapy. Although CAR-T cell therapy has made drastic progress in treating blood malignancies, yet it is often linked to serious systemic adverse effects, including neurotoxicity and Cytokine Release Syndrome (CRS) (ICANS). T cells generate a distinct, more potent collection of inflammatory cytokines, which trigger these effects.
On the other hand, the safety profile of CAR NK cell therapy is much better. NK cells are less likely to trigger potentially fatal systemic inflammation because they do not produce large amounts of interleukin-6 (IL-6), the primary cause of CRS. Furthermore, the risk of Graft-Versus-Host Disease is minimal since NK cells do not depend on T-cell receptors (TCRs) (GvHD).
This dampens the chances of weeks-long manufacturing delay needed for customized CAR-T treatments and enables "off-the-shelf" applications, where cells from a healthy donor can be used for numerous patients.
CAR NK Cell Therapy: Promise and Challenges in Solid Tumors
In the past, the dense, immunosuppressive environment of solid tumors has proven difficult for cell treatments to penetrate. Research conducted in 2024 and 2025 has focused on overcoming the "hostile" tumor microenvironment in the context of CAR NK cell therapy, especially in solid tumors (TME), exploring both its potential and challenges.
Lung, kidney, and ovarian tumors produce chemical and physical barriers that "switch off" immune cells. To counter this, scientists are now employing "logic-gated" technology, which enables NK cells to identify multiple markers simultaneously, ensuring that they target only cancerous tissue while protecting healthy stem cells.
The intrinsic capacity of NK cells to use both their native receptors and their modified CAR offers a dual-attack strategy that may prevent the "antigen escape" frequently observed in T-cell treatments, even though clinical data for solid tumors is still developing in comparison to blood malignancies.
Current Landscape: CAR NK Cell Therapy Clinical Trials
Clinical trials for CAR NK cell treatment have expanded into various medical specialties as of late 2025. This is now an experimental cancer therapy with wide-ranging systemic applications rather than just a cancer-focused project.
Hematological Success: Patients with B-cell malignancies and acute myeloid leukemia (AML) who had not responded to previous treatments have shown complete remission in recent Phase I/II trials.
Autoimmune Advancements: The success of CAR NK cell treatment for lupus is one of the biggest changes of 2025. In patients with severe, treatment-refractory Systemic Lupus Erythematosus (SLE), CD19-targeted NK cells have produced a "immune reset," resulting in a long-lasting remission with little adverse effects in limited clinical cohorts.
Viral and Regenerative Support: By eliminating damaged cells to make room for healthy tissue, NK cells are being used outside of oncology to manage viral infections and encourage tissue healing.
The Biology of the Natural Killer Cell
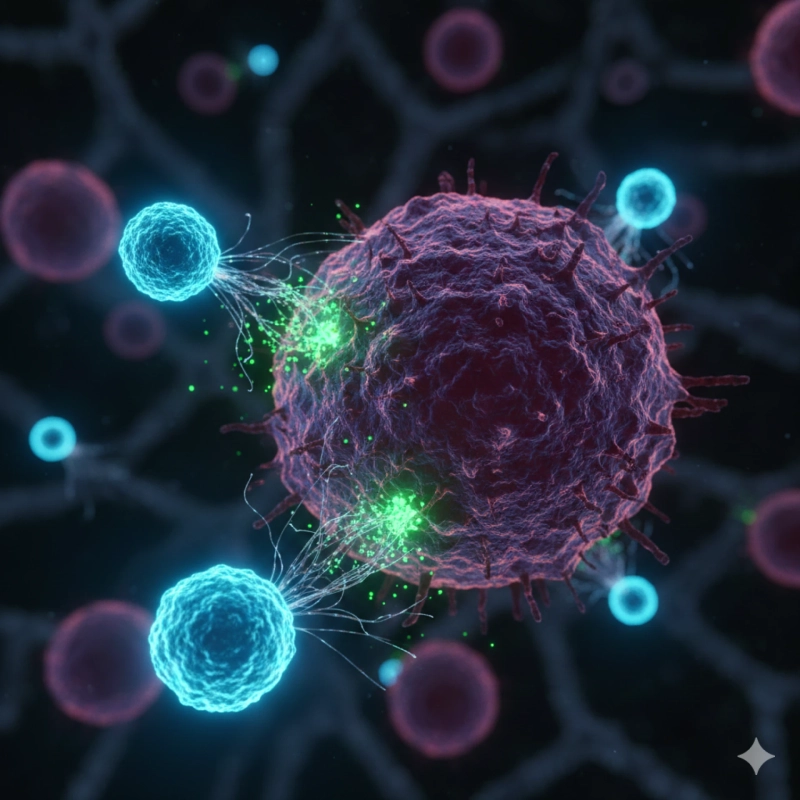
The innate immune system's first line of protection is provided by Natural Killer cells. NK cells naturally patrol the body to find and destroy aberrant cells, including those that are malignant or infected with viruses, in contrast to T cells, which need a particular antigen-recognition pathway to recognize a threat.
These cells evaluate targets in their natural form by striking a balance between activating and inhibiting signals. By downregulating their Major Histocompatibility Complex (MHC) class I molecules, cancer cells frequently try to avoid the immune system by becoming "invisible" to T cells.
However, NK cells are biologically programmed to detect this "missing self" signal, triggering the release of cytotoxic molecules like perforin and granzymes to induce rapid cell death.
How It Works: The Engineering of Precision
Although natural NK cells are powerful, CAR NK Cell Therapy uses genetic engineering to increase this power. Scientists provide these cells with a customized "navigation system" to locate specific proteins on a tumor's surface by equipping them with a Chimeric Antigen Receptor (CAR).
The development of these engineered NK cells typically involves several rigorous steps:
Isolation: NK cells can be isolated from peripheral blood, umbilical cord blood, induced pluripotent stem cells, and other sources (iPSCs).
Modification: The CAR gene is inserted utilizing viral vectors or CRISPR technologies to target specific markers like as CD19, CD33, or FLT3.
Expansion: The cells are cultivated in a controlled environment to reach therapeutic quantities, which usually fall between 1 and 5 million cells per kilogram of patient weight.
Timing Strategy: The infusion is frequently carefully planned to occur two weeks prior to or following traditional treatments like radiation or chemotherapy to maximize synergistic advantages.
Next Read: “Top NK cell Therapy companies to look for in 2026”
Accessing Advanced Care: Companies and Facilities
Patients frequently search for companies that bridge the gap between clinical research and patient access while looking for CAR NK cell therapy companies. Under the name Cancer Killer Cells offers these cutting-edge treatments in specific, controlled settings in Mexico, such as Cancun, Tijuana, and Nuevo Vallarta.
For those seeking focused cancer intervention and immune-boosting therapy outside the typical hospital bottleneck, these centers offer high-dose infusions and customized care programs.
Final Thought:
CAR NK cell therapy, which offers a quicker, safer, and more scalable substitute for earlier immunotherapies, is a turning point in medical history. This treatment offers a non-toxic approach to addressing some of the most challenging diseases of our time by harnessing the natural "killing" ability of NK cells and enhancing it through contemporary genetic engineering.
The potential for these cells to redefine wellbeing is just starting to become apparent, whether through the therapy of autoimmune illnesses, tumor killing, or cancer prevention.