Toxicological emergencies are an ever-present threat in both developed and developing nations. From accidental poisonings to drug overdoses and environmental hazards, the ability to swiftly counteract the effects of toxic substances can mean the difference between life and death. At the heart of these life-saving interventions lies the use of antidotes—agents specifically designed to neutralize toxins or mitigate their effects.
This guest post delves into the history, classifications, mechanisms, applications, innovations, and future prospects of antidotes, covering both clinical and research perspectives. Whether you are a healthcare professional, pharmaceutical researcher, or public health policymaker, understanding antidotes is critical to improving patient outcomes and public safety.
1. What Are Antidotes?
1.1 Definition
An antidote is a substance that can counteract a form of poisoning or toxic exposure. It works by neutralizing, reversing, or reducing the toxic effects of a particular poison or drug.
1.2 Purpose and Use Cases
- Accidental Poisonings (household chemicals, medications)
- Drug Overdoses (opioids, benzodiazepines)
- Occupational Exposure (pesticides, heavy metals)
- Bioterrorism and Warfare (nerve agents, cyanide)
- Environmental Toxins (carbon monoxide, snake venom)
2. History of Antidotes
2.1 Ancient Origins
- Charaka Samhita (India) and Hippocratic Writings (Greece) mentioned early antidotal formulations.
- Theriac: An ancient antidote used for multiple poisons, often a blend of dozens of ingredients.
2.2 Modern Pharmacology
- Discovery of specific antidotes began in the 19th and 20th centuries with the rise of pharmacodynamics and clinical toxicology.
- Introduction of naloxone in the 1960s marked a milestone in opioid overdose treatment.
3. Classification of Antidotes
TypeMechanismExamplesChemical AntidotesDirectly neutralize the poisonActivated charcoal, chelating agentsPharmacological AntidotesCounteract the effects via receptor antagonismNaloxone, flumazenilPhysiological AntidotesProduce effects opposite to those of the poisonAtropine, oxygenUniversal AntidotesGeneral agents used for a broad range of toxinsActivated charcoal (historically)Specific AntidotesTarget a single known toxinDigoxin immune Fab, N-acetylcysteine
4. Mechanisms of Action
4.1 Binding to Toxins
- Chelators: Bind heavy metals (e.g., EDTA for lead, dimercaprol for arsenic).
- Antibodies: Bind and inactivate specific molecules (e.g., digoxin immune Fab).
4.2 Receptor Blockade
- Naloxone binds to opioid receptors, displacing opioids and reversing respiratory depression.
4.3 Enzyme Activation
- N-acetylcysteine restores glutathione levels in acetaminophen poisoning.
4.4 Physiological Counteraction
- Atropine blocks parasympathetic activity, reversing effects of organophosphate poisoning.
5. Key Antidotes and Their Clinical Uses
AntidoteUsed ForMechanismNaloxoneOpioid overdoseOpioid receptor antagonistFlumazenilBenzodiazepine overdoseGABA-A receptor antagonistN-acetylcysteine (NAC)Acetaminophen toxicityReplenishes glutathioneActivated CharcoalVarious poisonsAdsorbs toxins in the GI tractAtropine + PralidoximeOrganophosphate poisoningAntagonism and reactivation of acetylcholinesteraseDeferoxamineIron poisoningChelation of iron ionsHydroxocobalaminCyanide poisoningBinds cyanide to form non-toxic complexesEthanol or FomepizoleMethanol/Ethylene glycol poisoningInhibit alcohol dehydrogenaseDigoxin immune FabDigoxin toxicityAntibody binding to digoxin
6. Routes of Administration
- Intravenous (IV): Fastest and most common in emergencies
- Oral: Used when immediate absorption isn’t critical
- Intramuscular (IM): Used in field conditions or pre-hospital care
- Inhalation: Used for gaseous antidotes like amyl nitrite
- Topical: For local venom neutralization or chemical burns
7. Challenges in Antidote Use
7.1 Limited Availability
- Not all hospitals have stock of rare or expensive antidotes.
- Supply chain issues can affect response in rural or resource-poor settings.
7.2 Diagnostic Uncertainty
- Time-critical decisions must often be made without complete toxicology panels.
- False positives/negatives in toxic screens can delay treatment.
7.3 Adverse Effects
- Some antidotes carry risks themselves (e.g., seizures with flumazenil).
- Hypersensitivity reactions (e.g., deferoxamine causing hypotension).
7.4 Cost and Accessibility
- Antidotes like digoxin immune Fab can cost thousands per dose.
- Fomepizole is expensive, limiting its use in low-resource settings.
8. Antidote Production and Regulation
8.1 Manufacturing Standards
- Pharmaceutical-grade production under GMP conditions.
- Stability testing for shelf life and storage (often refrigerated).
8.2 Regulatory Oversight
- FDA (US), EMA (Europe), CDSCO (India), and other agencies regulate approvals.
- Orphan Drug Designation for rare toxins (e.g., botulinum antitoxin).
8.3 Stockpiling Programs
- National antidote banks and strategic reserves exist in several countries.
- Example: CHEMPACK in the U.S. for nerve agent emergencies.
9. Antidotes in Bioterrorism and Chemical Warfare
- Soman, Sarin, VX Nerve Agents: Treated with atropine, pralidoxime, benzodiazepines.
- Cyanide Gas: Treated with hydroxocobalamin and sodium thiosulfate.
- Radiation Exposure: Potassium iodide to block radioactive iodine uptake.
Antidotes are an integral part of national defense and emergency preparedness protocols.
10. Research and Innovations
10.1 Monoclonal Antibodies
- Custom antibodies for rare drug overdoses and exotic venoms.
- Potential for targeted therapy with fewer side effects.
10.2 Nanotechnology
- Nano-antidotes designed for enhanced tissue penetration and selectivity.
- Used in animal models for snake venom and heavy metal detox.
10.3 Biosensors and Smart Antidotes
- Wearable devices that detect poisoning and deliver antidotes automatically.
- Still under development for diabetic ketoacidosis and opioid overdoses.
10.4 CRISPR and Genetic Rescue
- Potential for editing genes that are responsible for hypersensitivity to toxins.
- Long-term research focus in neurotoxicology and cancer therapy.
11. Public Health Perspective
11.1 Poison Control Centers
- Provide real-time guidance for antidote use.
- Reduce unnecessary emergency visits and optimize resource allocation.
11.2 Education and Awareness
- First responders, pharmacists, and the public benefit from training in antidote use.
- Naloxone distribution and training programs have saved thousands of lives.
11.3 Global Disparities
- Antidote availability varies significantly between countries.
- WHO and NGOs support global antidote banks and aid programs.
12. Case Studies
Case 1: Naloxone Saves Lives in the Opioid Crisis
A community naloxone distribution program in Ohio reduced opioid-related deaths by 25% within two years, proving the value of easy access and education in antidote distribution.
Case 2: Snakebite Treatment in India
Introduction of polyvalent antivenom in rural hospitals decreased mortality by over 50%, highlighting the importance of infrastructure and cold chain management.
Case 3: Cyanide Poisoning in Industrial Accident
Hydroxocobalamin administration to factory workers exposed to cyanide saved 18 lives with minimal side effects, emphasizing the need for on-site preparedness.
13. Future of Antidotes
13.1 Precision Antidotes
- Development of gene-specific or mutation-targeted therapies.
- Antidotes tailored for individuals with genetic sensitivities to toxins.
13.2 Open Access Databases
- AI-driven databases recommending real-time antidote therapy based on symptoms, lab results, and patient history.
13.3 DIY and Community Kits
- Portable kits for agricultural workers, outdoor enthusiasts, and caregivers of at-risk patients.
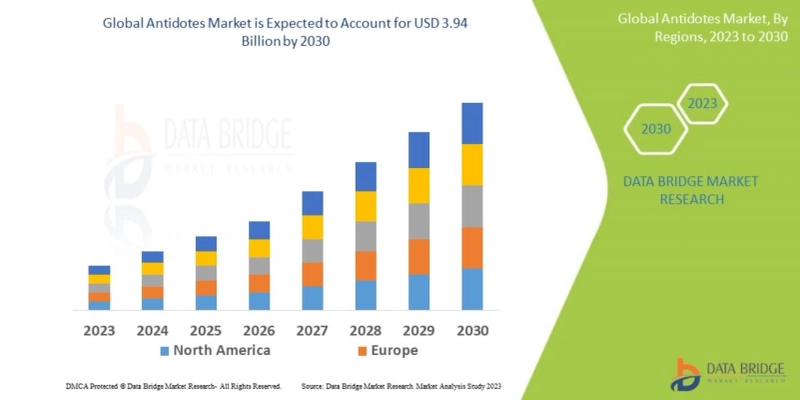
- Source: https://www.databridgemarketresearch.com/reports/global-antidotes-market
Conclusion
Antidotes stand as a critical pillar in emergency medicine, public health, and pharmacology. As the spectrum of toxic exposures continues to expand—from novel drugs to synthetic chemicals and environmental pollutants—the need for effective, accessible, and affordable antidotes has never been more urgent.
Collaboration between governments, healthcare providers, pharmaceutical companies, and communities is essential to ensure that antidotes reach every patient, regardless of geography or socioeconomic status. Whether on the battlefield, in a suburban home, or a hospital emergency room, antidotes remain a vital line of defense in saving lives.