A step-by-step guide for understanding the claims management process.
The technique used by insurance companies to analyze medical claims management systems for appropriate information, authentication, validity, and accuracy are referred to as the Medical Claims Management Process.
With the help of this procedure, the insurance company may reimburse the healthcare provider in whole or in part.
If the claim request is determined to be invalid, fraudulent, duplicated, or beyond the policy terms, the firm has all the right to reject it. Claim analytics and Disputes are handled with competent and expert legal counsels through medical claims management systems.
Despite such fraudulent medical claims management solutions scams, there is a potential for considerable improvements, emphasizing improved staff and patient experience, enhancing operations, and managing medical claims processing more effectively in terms of time and resources.
Before we get into the phases of medical claims management systems, it’s important to note that insurance companies aren’t eager to pay out claims, so they’ll seek any reason to prolong the process, especially if there’s missing information. Thus, any omissions in paperwork, unspecific restoration quotations, missing essential data, or incomprehensible claim forms should be avoided, as it may result in the claim being denied or the whole settlement process being delayed.
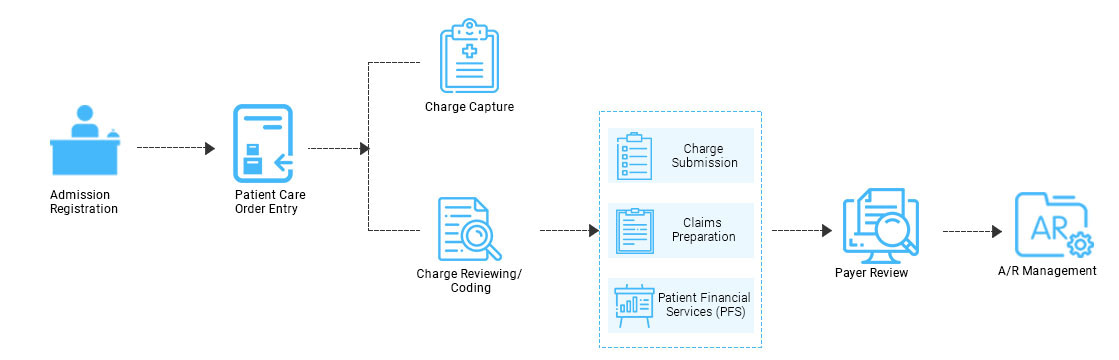
The claim analytics process primarily entails three critical steps. Let’s take a look at the medical claim process and why a smooth medical claims solutions process is so important:
-
Claims Adjudication:
The insurance providers review the following items on the list at this phase:
-
Pre-approval Grant.
-
Claim compatibility with the information provided in the pre-authorization request.
-
Reimbursement Eligibility of the patient.
-
Claim duplication Evidence.
-
Need to check if the hospital is on the list of authorized networks
-
Provision of Valid and Appropriate Treatment.
-
Evidence of medical therapy requirements.
-
Implementation of appropriate Medical coding.
-
Appropriate billing of each therapy included in the medication process.
For claim adjudication, insurance firms apply a fusion of computer-based and manual verification. It is followed by payment allocation, in which the insurance company determines how much it is inclined to pay for the claim.
2. Explanation of Benefits:
Once the adjudication procedure is over, the insurance provider then notifies the Caregiving institution, all about the facts and information of their determinations and justifications for paying or denying the claim. It is known as a benefits explanation or remittance assistance. The healthcare provider may give additional information or request that the claim be represented in terms of the amount reimbursed, amount authorized, permitted amount, patient accountability percentage, covered portion, discount portion, and so on.
3. Claims Settlement:
It is the concluding phase in this process wherein the insurance company covers the agreed sum to the healthcare provider for the service provided to the covered patient.
CONCLUSION:
It is critical to ensure that the necessary paperwork for the medical claims management process is completed so that the insurance provider may quickly pass the claim. It does relieve the patient of the responsibility of following up with the insurance company regularly.
In the scenario of a claim denial, the insured must determine the cause for the denial. If the justification is valid, it will not pay the claim. If the insured feels that the claim is accepted, then one might file a complaint with the insurance company’s grievance redressal cell.
Thus automated medical claim management systems enable seamless workflow throughout the claims life cycle, and It manages to combine numerous complex systems, platforms, and human procedures required.
