With the growth of virtual health practises such as telehealth and mHealth, it is more necessary than ever to manage bill payments and claims processing methodically. The medical billing cycle is a complex system comprised of numerous activities such as patient data management and medical record maintenance. Medical claims management is the foundation of healthcare insurance carriers since it demands customer commitment and data management. Healthcare providers may be compensated for their services provided through the medical claims process.
The quantity of documentation that medical claim solutions require can slow down medical professionals. Many healthcare claim management organisations are looking for strategies to reduce the inaccuracy and inefficiency of manually processing medical claims. However, this can be time-consuming and error-prone. Medical billing errors can have major consequences and have a negative influence on ROI generation. For all of these reasons, medical claims automation software is required. Processing medical claims automatically might help to speed up the billing process and decrease errors.
What is the process of processing medical claims through automation?
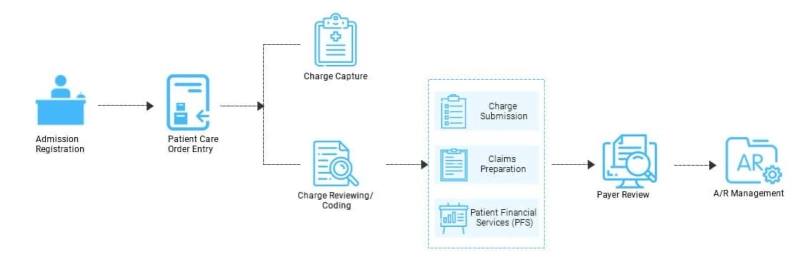
Medical claims processing software employs technology to conduct typical billing and claim management tasks. The automation of the medical claims processing cycle lowers data management errors and shortens the entire procedure. Healthcare providers and health insurance companies can employ claim processing automation to speed up activities such as patient onboarding, accounts payable, contract administration, and medical claims. In the healthcare business, EHRs that can capture and store health informatics as electronic records are employed in claim processing. Healthcare claims management software automates data entry, claim handling, and processing. The billing cycle using the programme is sped up in this method by automated medical claims processing.